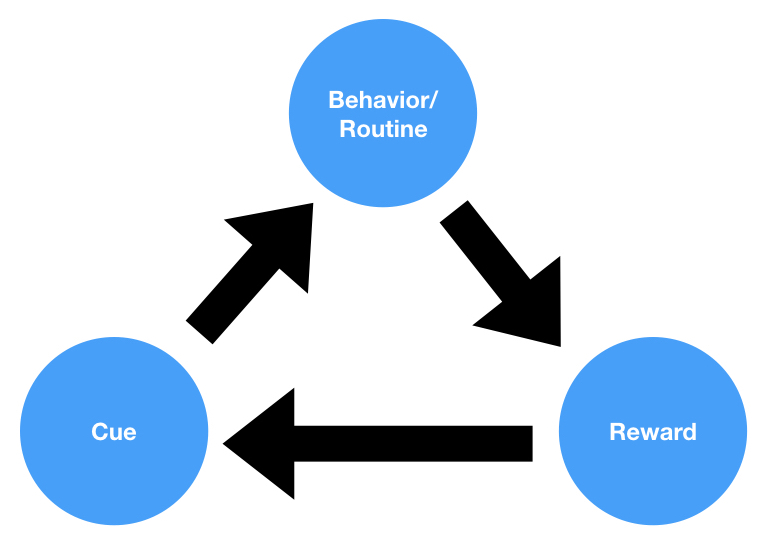
Whenever I talk about nudging, I get a barrage of messages about organ donation and how wildly successful nudging is at driving behavior-change in that domain.
I’ve long argued that organ donation defaulting is not actually an example of behavior-change in any commonly understood sense of the term. These programs are not actually getting people to *do* anything, they’re merely changing some laws to give governments the ability to do things to people.
This is why I think that if applied behavioral economics is good at one thing, it’s public relations. The field is full of people who are good at coining new terms and playing impressive rhetorical games.
Well, in the case of organ donation defaulting, it also turns out that these programs are also just not very effective. Not only are these programs not changing behavior, but they’re also not driving very impressive organ donation numbers.
According to a paper published in 2019, opt-out vs. opt-in organ donation systems are basically equal when it comes to organ donation rates. Here are few key quotes from the paper:
“Our study findings suggest no significant gain for established opt-in countries considering a switch to optout. Although historically some countries have observed impressive increases after introduction of presumed consent, such as Belgium, others have fared badly with either no difference or an actual drop in organ donation rates, including Singapore, Brazil, Chile, Sweden, and more recently Wales.”
“Comparing opt-out with opt-in countries we observed no significant difference in total deceased donor rates (20.3 vs. 15.4, respectively; P = 0.195), but there were significantly less living donors (4.8 vs. 15.7, respectively; P < 0.001) among opt-out countries (Table 3).”
“Although numerically opt-out versus opt-in countries appeared to have more deceased donor kidney transplants, this was not found to be statistically significant (30.3 vs. 23.4, respectively; P = 0.134). However, we did observe significantly less living donor kidney transplants among opt-out versus opt-in countries (4.5 vs. 15.2, respectively; P < 0.001). Altogether, there was no difference in overall kidney transplantation rates between opt-out versus opt-in countries (35.2 vs. 42.3, respectively; P = 0.405).”
“There was no significant difference in overall rates of liver transplantation between opt-out versus opt-in countries. However, although no significant differences were found in deceased donor liver transplantations (13.0 vs. 10.2, respectively; P = 0.483), opt-out countries had a significantly lower rate of living donor liver transplantation (0.0 vs. 0.6, respectively; P = 0.025). No significant differences were observed with other solid organ transplants, including heart, lung, pancreas, or small bowel. We observed no significant difference in total transplantation rates between opt-out versus opt-in countries when overall nonrenal (28.7 vs. 20.9, respectively; P = 0.606) or overall solid organ transplantation activity was analyzed (63.6 vs. 61.7, respectively; P = 0.909).”
Crazy, isn’t it? I bet you didn’t hear these results in the press.
That seems to be the story with social psychology and behavioral economics in general–lots of flashy headlines when surprising things are discovered, but basically no coverage when those things turn out to be untrue.
Just last year, a nice overview and analysis of the state of organ donation programs came out, linked here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8128443/
The author does a comprehensive job of covering the different types of organ donation programs and assessing their pros and cons. Here’s a nice table from the paper showing the impact of changing to an opt-out (organ donor by default) system:

As the author summarizes: “Through this review of recent literature, several trends start to emerge that define successful donation policies (Table 1). Firstly, there is no numerical consensus on which donation system (opt-in or opt-out) is superior. Secondly, successful system changes are accompanied by complementary interventions at different levels of society and the health system. Thirdly, legislative adaptation and flexibility is essential.”
As you read through this paper and learn about the countries that have successful organ donation systems, you quickly realize that a lot of stuff needs to be implemented in order for a system to work. It’s not a simple, quick change to the default (organ donor vs. non-donor). For example, Spain, which has the highest deceased donation rate worldwide, has invested a tremendous amount of time and money into optimizing its organ donation program from the ground up. The author of the above paper lays things out well:
“The Spanish government established a national transplant network across all hospitals, and invested substantially in facilitating the early identification of potential donors by capacitating hospital staff specifically for this purpose. A vast transplant coordinator network, specially trained in requesting organ donation, approaches family members. There has been a drive to promote donation after circulatory death, as well as the use of expanded criteria allografts to increase organ utilisation. These factors are thought to have had much more impact on deceased donation rates than the overall organ procurement system.
The case of Spain also teaches us about the importance of nuance in assessing organ donation systems, and the potential danger of labelling a system as one thing, or another. Spain conforms to the traditional premises of neither organ donation system – but perhaps is more similar to opt-in, than opt-out. Effectively, this distinction between systems does not seem as important as the careful layers of legislation, public education, healthcare infrastructure and human resourcing that have been instituted in Spain. Barriers to transplant were identified within the Spanish context, and systematically addressed. Although relativism is to be discouraged, a multifocal approach that is specifically tailored the transplant context of a country, and can respond to change, appears to have significant benefits.”
As you can see, Spain is more of an opt-in than an opt-out system, and they’ve done a ton of other stuff to make the system work. Anyone telling you that defaults are what makes all the difference either doesn’t know what’s going on in the real world, or they’re lying to you.
So the next time someone tells you that behavioral economics nudges are powerful tools for changing behavior, point them to my earlier piece linked here.
And if they tell you that organ donation rates actually prove that nudges are a roaring success, send them this article.
I’ll leave you a couple of final paragraphs from the author of the organ donation review article (emphasis mine):
“What lessons can be learnt from this extensive analysis? Firstly, there does not seem to be a single country where an increase in deceased donor numbers can be simply attributed to a change in donation system.13–15,22,47 In fact, a change in system from opt-in to opt-out, without accompanying changes addressing public education, awareness and health system structures has resulted in lower donation rates, for instance in Brazil. Moreover, those countries that are heralded as barometers of a successful opt-out system may not be so – like Spain. It is also notable that hard opt-out systems have not gained public acceptance and a conversation with potential donor families is still required. Hence, barriers to donation that manifest at the bedside of the deceased during this period, are not likely to fall away.
Rather, the success of organ donation policies seems to depend on clear communication, which is reinforced by extensive government buy-in and a willingness to readily respond to public sentiment should the need arise. Widespread investment in human resource infrastructure is needed at hospital level, with people capacitated to have difficult conversations with families and to identify potential donors. Technical support, with the capacity to maintain donor registers and transplant waiting lists, is also essential. Furthermore, these mechanisms need to be accountable through diligent reporting of verified data that are made public. This boosts public trust in the transplant system by demanding accountability and transparency – vital elements of successful organ donor programmes.”